MATERNAL AND CHILD HEALTH CERTIFICATE
Module 1: Unique Barriers to Health Care for Women
Introduction
Why don't people seek health care services when in need and when care is available? The answer to this question is multifold, and it is important to note that lack of awareness about treatment availability and benefits is not the primary issue.(1) Rather, patients face a variety of barriers that combine to prevent them from seeking proper medical attention. These barriers to care include cost, fear of doctors and treatment, cultural beliefs about fatalism, and lack of transportation, among others.
While many people in low- and middle-income countries face these challenges, women disproportionately bear the burden of health inequalities across the globe and are presented with unique barriers to accessing medical care. For example, women and children are disproportionately affected by transportation barriers, which may arise in the form of geographical isolation, lack of public transportation, lack of childcare, or lack of funds to purchase their own mode of transportation.Women are also more likely to work in the informal sector doing informal activities, domestic work, or unpaid family work. 90% of employed women in Africa work in the informal sector, limiting their access to the health insurance or social protection that a formal job often provides. This increases the financial burden of healthcare, since all costs have to then be paid out of pocket. Even when the family can afford the health care costs, cultural norms might prevent women from having control over how the family's money is spent, leaving financial decisions to the husband or male head of the household.(2)
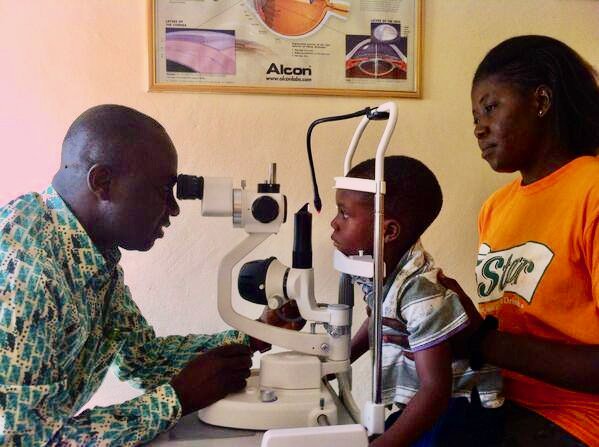
Examples from Eye Care
Although blindness in the developing world is oftentimes curable, many patients do not receive medical attention. One recent study found that “over two thirds of adults over age 40 in a rural Indian population with low vision secondary to cataracts, glaucoma, and refractive error had never sought eye care,"(3) while another study showed that "90 % of the people seeking eye care in poverty-stricken areas in Sri Lanka had similarly had no previous eye care."(4)
The 2019 Global Burden of Disease analysis, led by the Institute for Health Metrics and Evaluation, found that women account for 27% more of the older adults with vision loss than men do. Even after accounting for different demographics "women still had an 18 percent larger share of the burden of cataracts and a 23 percent larger share of the burden of uncorrected refractive errors compared to men."(5) In fact, females of all ages (including children) are more frequently exposed to causative factors, like infectious diseases and malnutrition, and utilize eye healthcare services less often than men.(6) In 2019, women had a 26% higher prevalence of blindness from cataracts, up from 13% higher in 1990.(7)
Why do these drastic inequalities exist? On the surface, there are proximate factors that contribute to health disparities between men and women, such as lower levels of education, literacy, and socioeconomic status. Yet underlying these proximate factors are the ultimate causes of gender inequality. Socially embedded constructs of masculinity, power differentials, and social status are all fundamental factors that manifest in poor health outcomes for women and constrain their ability to access medical care.
Proximate Factors
As discussed, many studies reveal that women receive eye care at a lower rate than men, despite a higher prevalence of eye diseases.(8)(9) Proximate reasons cited for this difference include lower literacy rates among women (10) and the fact that "poor rural women often have less disposable income, or control of finances, than men."(11) In fact, "female literacy remains the strongest independent predictor of health service utilization by women themselves and of the overall population, across all socioeconomic levels."(12) Public health interventions in Southern India have shown that an indirect investment in female education improves all aspects of health, including an increase in the use of already available health services.(13)
Another reason why women may not seek corrective surgeries is the expectation that they stoically persevere through adversity. One study found "that men were more likely than women to adopt a 'sick role.'" In contrast, women were more likely to continue their routines through adversity instead of emphasizing the need for surgery.
Ultimate Factors
While lower levels of education, literacy, and income are proximate reasons for gender disparities in eye health, the root cause can be traced to the low social status of women in much of the Global South. In order to reduce gender disparities, the ways in which social status impacts health must be understood. The inferior social status of women may increase their susceptibility to disease through a mechanism of dependency, vulnerability, and lack of opportunity. These social realities are the result of larger power differentials embedded within the community. A low social status means that women often do not have the same privileges and "rights" as men. In such an atmosphere, women may have less of an ability to assert themselves, a major impediment to accessing healthcare.
Because of these ultimate and proximate factors, the many barriers that impoverished individuals face in accessing care—such as transportation, money, and stigma—are raised higher for women. For example, the amount of time that a woman can spend travelling to get medical care is dependent on her unique social role. Because women are often the primary caretakers, they must find ways to navigate the obligations of childcare and household duties in order to walk to a health facility.(14) Safety concerns and cultural norms can also prevent women from traveling alone to seek medical care.(15) Similarly, a woman's financial access to care may depend not only on household resources but also on her societal value. If her husband or relatives decide that it is not worth spending the money, then a woman lacks financial access to care.
“Cultural obstacles to accessing health care are many and powerful. Woman and girls are often sent to cheaper traditional healers rather than Western medical providers. They may be discouraged or forbidden from leaving the house, even for medical care. They may not be allowed to see male health care providers, even if female providers are not available.” (15)
A study looking at barriers to healthcare for women in Myanmar found that women experience fewer barriers and are more likely to seek healthcare if they are empowered. If women are educated and empowered on how to advocate for themselves they are more likely to use contraception and have more time in between child births. Myanmar census data showed that "62% of maternal deaths occurred at home and 14% occurred on the way to the hospital due to late referrals, primary delays, and long travel distances." The barriers to care that lead to these high maternal death rates are reduced when women are empowered.(16)
Conclusion
Within the fields of epidemiology, anthropology, sociology, and public health, the unique problems that women face are familiar and well-conceptualized. Yet despite the understanding and academic consensus around the issue of women's vulnerability to infectious and chronic diseases, the problem remains virtually untouched in the policy world. In other words, understanding about the issue has not translated into a solution. The reality that women in low- and middle-income countries are not only victimized by poor health, but also by societal conditions that can make it impossible for women to be in control of their health, poses major challenges for policy makers. In this situation, it seems that the largest impediment to action is complexity. As Bill Gates remarked in a Harvard commencement address, "the barrier to change is not too little caring; it is too much complexity. Yes, inequity has been with us forever, but the new tools we have to cut through complexity have not been with us forever. They are new - they can help us make the most of our caring - and that's why the future can be different from the past."(16)
Footnotes
(1) Donoghue, M. " People Who Don't Use Eye Services: 'Making the Invisible Visible.'" Journal of Community Eye Health. 12.31 (1999): 36-38.
(2) Parmar, D., Victora, C., Barros, A., Ewerling, F., Heidari, S., & Magar, V. (2019). Breaking Barriers: Towards more gender-responsive and equitable health systems. In P. Salama, & S. Asma (Eds.), In: Primary Health Care on the Road to Universal Health Coverage. 2019 Global Monitoring Report World Health Organization (WHO). https://www.who.int/healthinfo/universal_health_coverage/report/2019/en/.
(3) Chang, M.A., Condon, N.G., Baker, S.K., Bloem, M.W., Savage, H. and Sommer, A. "The surgical management of cataract: barriers, best practices, and outcomes." International Ophthalmology. 28.4 (2008): 247-260.
(4) Holden, B.A. "Blindness and Poverty: A Tragic Combination." Clinical and Experimental Optometry. 90.6 (2007): 401-403.
(5) Steinmetz, J., et al. "Staring Down Gender Disparities in Vision Loss." Think Global Health, 19 Feb. 2021, www.thinkglobalhealth.org/article/staring-down-gender-disparities-vision-loss.
(6) Seva Canada Society, and Seva Foundation. Gender and Blindness: Initiatives to Address Inequity. Rep. 2008. https://www.seva.org/site/DocServer/Gender_and_Blindness.pdf;jsessionid=00000000.app20014a?docID=483&NONCE_TOKEN=6A573A1E5BC9D36F255946FF719FEE8E.
(7) Steinmetz, J., et al. "Staring Down Gender Disparities in Vision Loss." Think Global Health, 19 Feb. 2021, www.thinkglobalhealth.org/article/staring-down-gender-disparities-vision-loss.
(8) Lewallen, S. and Courtright, P. "Gender and use of cataract surgical services in developing countries." Bulletin of the World Health Organization. 80.4 (2002): 300-303.
(9) Chang, M.A., Condon, N.G., Baker, S.K., Bloem, M.W., Savage, H. and Sommer, A. "The surgical management of cataract: barriers, best practices, and outcomes." International Ophthalmology. 28.4 (2008): 247-260.
(10) Ibid.
(11) Lewallen, S. and Courtright, P. "Gender and use of cataract surgical services in developing countries." Bulletin of the World Health Organization. 80.4 (2002): 300-303.
(12) Courtright P, West SK, Contribution of Sex-linked biology and gender roles to disparities with trachoma. Emerging Infectious Diseases. 2004;10:2012-2016.
(13) Nirmalan PK, Padmavathi A, Thulasiraj RD. Sex inequalities in cataract blindness burden and surgical services in south India. Brit J Ophthal. 2003;87:847-849.
(14) Seva Canada Society, and Seva Foundation. Gender and Blindness: Initiatives to Address Inequity. Rep. 2008. https://www.seva.org/site/DocServer/Gender_and_Blindness.pdf;jsessionid=00000000.app20014a?docID=483&NONCE_TOKEN=6A573A1E5BC9D36F255946FF719FEE8E.
(15) Htun, N.M.M., Hnin, Z.L. & Khaing, W. Empowerment and health care access barriers among currently married women in Myanmar. BMC Public Health 21, 139 (2021). https://doi.org/10.1186/s12889-021-10181-5.
(16) Ibid.
(17) Seva Canada Society, and Seva Foundation. Gender and Blindness: Initiatives to Address Inequity. Rep. 2008. https://www.seva.org/site/DocServer/Gender_and_Blindness.pdf;jsessionid=00000000.app20014a?docID=483&NONCE_TOKEN=6A573A1E5BC9D36F255946FF719FEE8E.
(18) Gates, B. Address at Harvard, June 7, 2007. Innovations (2)4:2007.
