MATERNAL AND CHILD HEALTH CERTIFICATE
Module 3: Reproductive Health and Family Planning
The Problem
Achieving good reproductive health remains a far-off goal in many parts of the world. This lack of care has repercussions. An estimated 830 women die of pregnancy-related causes each day, amounting to more than 300,000 deaths each year; 99% of these deaths occur in low- and middle-income countries.(1) However, access to family planning can greatly reduce these mortality rates. One 2012 study found that contraceptive use caused a 44% reduction in maternal mortality in 2008; these researchers also predicted that providing access to contraception for all those who need it would reduce worldwide maternal deaths by 29%.(2) These statistics call for increased access to reproductive health and family planning services.
What is Reproductive Health and Family Planning?
Reproductive health is a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity, in all matters relating to the reproductive system and to its functions and processes.”(3) Family planning is one of the most basic and essential healthcare services that can promote and ensure reproductive health, yet 12% of women in most regions of the world have an unmet need for family planning.(4)
Family planning can reduce maternal mortality by preventing unwanted pregnancy and unsafe abortion and by promoting healthy pregnancies.(5) Enabling couples to determine whether, when, and how often to have children is crucial to safe motherhood and healthy families. For example, family planning has profound health, economic, and social benefits:(6)
Protecting the health of women by reducing high-risk pregnancies;
Protecting the health of children by allowing sufficient time between pregnancies;
Fighting HIV/AIDS through providing information, counseling, and access to male and female condoms;
Reducing abortions;
Supporting women's rights and opportunities for education, employment, and full participation in society;
Protecting the environment by stabilizing population growth.
Introduction to Contraception
How Pregnancy Occurs(7)
The average menstrual cycle lasts 25 to 30 days. Following menstruation, hormones (chemical signals in the body) cause eggs in the ovaries to mature and subsequently triggers the uterine lining to thicken. Halfway through the menstrual cycle, a rapid increase in levels of certain hormones causes one mature egg to leave an ovary (ovulation) and travel through a fallopian tube toward the uterus, while the uterine lining continues to build up. When a woman has vaginal intercourse, sperm from the male’s ejaculate travel into the vagina, through the uterus, and into the fallopian tubes, where fertilization may occur. Fertilization is most likely to happen when a woman has intercourse during the five days prior to ovulation or on the day of ovulation. If a fertilized egg implants in the wall of the uterus, pregnancy occurs. If the egg is not fertilized or a fertilized egg does not implant in the uterine wall, pregnancy does not occur, and the uterine lining breaks down and is excreted (menstruation).
How Contraceptives Work(8)
Contraceptives prevent pregnancy in a variety of ways: preventing sperm from entering the female reproductive tract, preventing viable sperm and oocytes (eggs) from meeting, and preventing ovulation and thickening cervical mucus.
Methods that prevent sperm from entering the female reproductive tract:
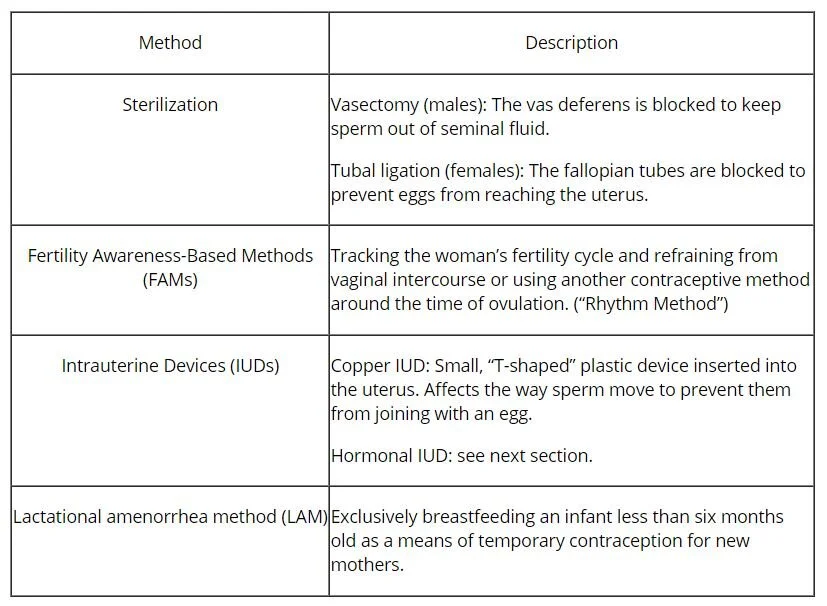
Methods that prevent viable sperm and oocytes from joining:
Hormonal methods of contraception:
Hormonal contraceptives contain synthetic versions of the hormones usually produced by a woman’s ovaries. Combined hormonal contraceptives contain estrogen and progestin, while some contraceptives contain only progestin. These hormones suppress the release of other hormones required for ovulation. This also suppresses the growth of follicles, the structures within the ovaries in which a woman’s eggs mature prior to ovulation. When ovulation is prevented, an oocyte is not released from the ovary and cannot encounter sperm, thereby preventing pregnancy. In addition, progestin signals the woman’s cervix to produce thicker mucus, which makes it more difficult for sperm to move from the vagina into the uterus.
Effectiveness of Different Contraceptive Methods(9)(10)(11)
Contraceptive Usage Patterns
Although worldwide contraceptive use has increased over the past few decades, there remains a large unmet need for contraception, particularly in low- and middle-income countries.(12) The World Health Organization estimates that 214 million women of reproductive age in low- and middle-income countries would like to stop childbearing but are not using contraception; the Guttmacher Institute reports that of the more than 50% of women of reproductive age in low- and middle-income countries who want to avoid pregnancy, 17% are not using any method of contraception.(13)(14) Sub-Saharan is the region with the highest level of unmet need at 24%.(15) On average, the poorest women are four times less likely to use contraception than the wealthiest women.(16) The unmet need for contraceptives has enormous implications for maternal health: the number of maternal deaths could be reduced by 29% if all women and men had access to contraception to prevent unwanted pregnancies.(17)
Use of certain methods of contraception is influenced by personal preference, by the availability of methods, and by the cost and consistency of methods.(18) Variability is found in the Global North and the Global South:
Oral birth control pills are used by 27% of married contraceptive users in Bangladesh but only 3% of those in India, where 37% of married contraceptive users use sterilization methods.(19)
Intrauterine devices (IUDs) are used by 36% of married contraceptive users in Egypt and 41% of married contraceptive users in China. That figure drops to 0.3% in Sudan and to 5% in the United States, where female sterilization (24%) and oral contraceptives (16%) were the most commonly used methods of contraception from in 2013.(20)
Factors Affecting Contraceptive Use
Patient and Provider Beliefs
Patient and provider beliefs differ drastically between communities and cultures and strongly influence patterns of contraceptive use.(21) In a 2010 study of the Mityana and Mubende districts in Uganda, focus group discussions with people between the ages of 15 and 24 revealed a variety of misconceptions about contraceptives, including the belief that condoms can damage the uterus and even cause death. Many women in the study explained that discussing contraception with their male partners was considered “unacceptable” and that their efforts to initiate such discussions were ineffective.(22) In 2011, semi-structured interviews with 102 contraceptive providers in the same region revealed that most providers had “negative attitudes towards the provision of contraceptives to young people [and] imposed non-evidence-based age restrictions and consent requirements.” The providers’ opinions about contraception, such as the belief that contraceptive can cause female infertility, negatively affected their willingness to distribute contraceptives, particularly to young unmarried women.(23) In interviews with 93 pharmacy employees in Managua, the capital of Nicaragua, only 65% of providers reported that they were willing to provide emergency contraceptives to “all women in need,” and only 13% of providers said that they would provide emergency contraception to minors.(24)
Long-lasting contraceptives such as subdermal implants, injections, and IUDs are often underused because of limited availability, misconceptions about health risks, and a lack of qualified personnel. However, a study in Kenya found that when implant technology is available, it is welcomed by many women and is more effective in preventing pregnancy than short-acting methods of contraception. In a study of almost 400 young Kenyan women, 24% of participants chose an implant over short-acting contraception, and the occurrence of unintended pregnancy was significantly less in the long-acting contraceptive group. Over the course of the 18-month study, the probability of discontinuation was significantly greater in the short-acting contraceptive group; only 19% of implant users chose to stop using the method, compared to 65% of the short-acting contraceptive group.(25) Similarly, a study in North Ethiopia found that Depo-Provera, a long-term hormonal birth control injection, was found to be the most utilized contraceptive method by women. (26)
Misinformation has also led to limited use of long-acting contraception in the Global North. In the United Kingdom, where long-acting contraceptives are underused, focus groups in two cities in Scotland revealed that the majority of women held “firm but incorrect beliefs about [long-acting reversible contraception’s] safety and side effects [and] disliked any method which involved an invasive procedure and/or vaginal examination.” Interestingly, providing participants with accurate information about long-acting contraceptive methods following the initial group discussion “was not wholly successful in dispelling negative views” about those methods, whereas oral contraceptives and condoms were “familiar and acceptable” to most women.(27)
Male Attitudes Towards Contraception
Male attitudes towards contraception strongly influence the willingness and ability of women to use contraception. Ten percent of married women with unmet need for contraception in Latin America and the Caribbean, along with 22-25% of married women with unmet need in Sub-Saharan Africa and Asia, do not use contraception because “their husbands or someone else close to them oppose the use of contraceptives.”(28) This poses an enormous challenge to women in Sub-Saharan Africa, where spousal consent for females to receive contraceptives is often required by health care providers.(29) For instance, in Republic of the Congo, many clinics and hospitals provide women with contraceptives only if their husbands are present.(30)
Attitudes Towards Menstruation
Female attitudes towards menstruation and fertility, which strongly influence contraceptive use, vary widely among women. While amenorrhea (absence of menstruation) is still considered unacceptable by many women, a preference for infrequent menstruation or amenorrhea has increased in recent years. A 2003 study of over 1,000 women attending family-planning clinics and almost 300 contraceptive providers in China, South Africa, Nigeria, and Scotland found that, with the exception of black women in the African clinics, the majority of women disliked their period, citing “inconvenience” as the primary reason. Even among women in Africa who preferred monthly menses, the majority of all women surveyed responded positively to trying a method of contraception that would temporarily induce amenorrhea.(31)
A 1999 study in the Netherlands used telephone interviews to investigate attitudes of Dutch women towards menstrual bleeding patterns. Only a third of women of reproductive age preferred monthly bleeding, and the majority of women between the ages of 15 and 49 preferred bleeding less than once a month or amenorrhea.(32) Similar attitudes towards menstruation have been reported among urban women in India. One study found that 80% of urban women surveyed (high school and college students and professional women) wanted “infrequent menses or no menses at all”. This was in sharp contrast to rural Indian women (housewives working on family farms), of whom 70% preferred monthly menstruation and viewed it as a necessary, natural event.(33) The recent increase in positive attitudes towards amenorrhea and reduced frequency of menstruation suggests that health care providers should be cognizant of changing female attitudes towards menstruation and the acceptability of different methods of contraception.
Access to Contraceptives(34)
General Barriers to Access
Women in many communities face significant barriers to contraceptive access, with at least 9-15% of married women in low- and middle-income countries reporting that they “do not have access to contraceptives, cannot afford them, or do not know about them.”(35) Women using short-term contraceptives must return frequently to their providers to obtain their next dose. The difficulty of finding transportation, the financial cost of travel and of contraceptives, and the travel time (taking away from child-rearing and work) make consistent visits to clinics a challenge for many women in low- and middle-income countries. Furthermore, although oral contraceptives and hormonal injections are popular in many regions in the Global South, particularly in Africa, effective use of these methods is constrained by limited supplies at clinics.(36) For instance, in a study conducted from August 2008 to February 2009 in the Mityana and Mubende districts in Uganda, female condoms, combined hormonal dermal patches, vaginal rings, cervical caps, spermicides, diaphragms, monthly injections, and hormonal IUDs were not available in any of the 102 public, private non-profit, and private for-profit health facilities studied, and most providers were not medically competent to provide long-acting contraceptives. In addition, contraceptive use was limited by “sporadic contraceptive stocks, poor service organization, [a] limited number of trained personnel, high costs, and unfriendly service.”(37) Even without barriers to physical access of contraceptives, utilization can still be quite low. A study of men and women in health zones of the DRC with strong access to family planning found that the main barriers to contraceptives include fear of sterility, costs, cultural norms, family pressure to avoid contraceptives, and a lack of information. (38)
Governmental policies regulating contraceptive access(39)
Although governmental policies regulating contraceptive use vary, 91% of all countries supported family planning programs and contraceptives by 2001, either directly (through government facilities) or indirectly (by supporting non-governmental agency activities). Low- and middle-income countries tend to have greater direct government support of family planning, while countries in the Global North have shifted towards indirect support of contraception. The majority of African countries directly support the distribution of contraceptives; Somalia, Cameroon, Central African Republic, Chad, and Sierra Leone offer indirect support. In Eastern Asia and Oceania, 80% of countries directly support contraceptive distribution and 13% offer indirect support, while Brunei, Laos, and Turkmenistan provide no support. In Western Asia, 88% of countries support contraceptive access, although Oman and the United Arab Emirates provide no support. By 2001, all countries in Central and South America provided direct support for contraception access, except for Argentina and Belize. The majority of governments in Europe and North America offer direct support for contraceptives, although Andorra, Germany, Greece, Italy, Slovakia, and Switzerland provided no governmental support as of 2003. However, the success of governmental policies supporting contraception depends on sufficient funding, program implementation, cultural attitudes, civil conflict, and existing health care infrastructure, among other factors.
Contraceptive access in the United States
Since 2010, 28 U.S. states required insurers covering prescription drugs to cover all FDA-approved prescription contraceptive drugs.(40) The Affordable Care Act, the health care reform bill passed by the Obama administration in 2010, required insurance companies to fully cover all contraceptive methods approved by the FDA, in an attempt to remove financial barriers to birth control access.(41) However, the law was strongly opposed by religious and conservative groups and was subsequently reviewed by the United States Supreme Court, which ruled that the bill was constitutional in June 2012.(42) The future of contraceptive coverage is unclear under the Trump Administration, which is attempting to roll back the birth control mandate. (43)
In the U.S., oral contraceptives are currently only available by prescription, with the exception of some emergency contraceptives, and there is growing debate over whether to make oral contraceptives available over the counter. The Oral Contraceptive Over-the-Counter Working Group, a women’s health clinical and research institution, argues that requiring prescriptions to access oral contraceptives is “patronizing to women, limits contraceptive freedom, and is ineffective against intractably high teen-pregnancy rates.” The group reports that teenagers’ access to birth control is particularly limited since it is more difficult for them to seek prescription-based contraceptive services without a parent’s help. The group is currently working to get over-the-counter approval for progestin-only pills, which may have fewer side effects than combined hormonal contraceptives.(44) Although 68% of women surveyed in one study were in favor of an over-the-counter contraceptive option, some health providers worry that making birth control available without requiring a meeting with a medical professional might result in negative health consequences for women, including unintended pregnancies resulting from incorrectly used birth control. In addition, although interest in over-the-counter oral contraceptives was highest among women who were uninsured, there is concern that an over-the-counter option could make birth control unaffordable for women on federal programs like Medicaid, which may not cover all over-the-counter drugs.(45)
Recent Developments in Contraception
Use of Emergency Contraception
Emergency contraception (EC) is a method of contraception designed to prevent unintended pregnancies in “emergency situations,” such as when no contraceptive was used during intercourse, or following contraceptive failure or incorrect usage, or in cases of sexual assault. According to the World Health Organization, emergency contraception can prevent 95% of pregnancies if taken within 5 days after intercourse.(46) EC pills currently on the market contain estrogen and progestin or only progestin, and the pills are taken in two phases or in a single dose, typically within a few days after unprotected intercourse. Like other hormonal contraceptives, EC pills inhibit or delay ovulation or prevent fertilization.(47) Copper IUDs, mifepristone, and ulipristal acetate (Ella® in the U.S.) are also available as emergency contraceptives in a number of countries.(48) The World Health Organization reports that emergency contraceptives are not appropriate for regular use. Although repeated EC use has not been associated with health risks, ECs have a higher failure rate than modern contraceptives designed for regular use, resulting in increased pregnancy risk when ECs are used as the primary contraceptive method.(49) The emergency contraceptive Ella® has a 2.1% failure rate if taken within 120 hours after intercourse and Plan B® reduces the risk of pregnancy by 81 to 90 %, whereas daily oral contraceptives and long-lasting hormonal methods have a failure rate of less than 1%.(50) Although emergency contraceptives are primarily available in pill form, researchers are exploring other modes of delivery. Current research is being conducted to determine whether a single vaginal administration of synthetic progestin via Carraguard gel, a non-contraceptive microbicide gel used to prevent transmission of sexually transmitted infections and HIV, might be an effective emergency contraceptive method.(51)
Worldwide use of emergency contraception is low relative to that of most other modern contraceptive methods, but usage varies by country. As of 2017, emergency contraceptives were available without a prescription in 95 countries, and 147 countries had registered an emergency contraceptive product.(52) Despite this, many low- and middle-income countries still have low rates of EC use and knowledge among women of reproductive age. The percentage of women who have knowledge about emergency contraception ranges from 3% in East Timor to 45% in the Dominican Republic; in comparison, 99% of women in Spain had knowledge of EC.(53) The percentage of women of reproductive age who had ever used or were currently using emergency contraception is even lower; only 0.3% in Haiti, 0.2% in Mali, and 0.1% in Nepal have ever used emergency contraception.(54)
Prevalence of emergency contraceptive use has increased rapidly in some regions, although this growth is partially attributable to an increased reliance on EC as a primary method of contraception. This phenomenon is particularly apparent among educated independent women in India, where sales of EC pills have surpassed sales of condoms and other oral contraceptives. It is hypothesized that the adoption of oral contraceptives intended for regular use has been slow due to a historical emphasis on female sterilization and the success of large advertising campaigns by EC manufacturers.(55) A similar usage pattern has emerged in Nicaragua, where many young unmarried women do not seek contraceptive health services out of fear of societal repercussions; Nicaraguan society often disapproves of premarital sex for women, and abortion is illegal in Nicaragua. Instead, many women turn to over-the-counter emergency contraceptives to prevent pregnancy. In 2006, nearly 50% of sexually active young women in Managua, Nicaragua who were not pregnant and did not have children had never used any method of non-emergency contraception, but interviews with 93 pharmacy employees in Managua showed that 92% of providers sold emergency contraceptive pills at least once a week.(56)
In the United States, the emergency contraceptive Plan B® was approved for over-the-counter sales in 2006 for women over the age of 18. Brand name and generic forms of emergency contraceptives such as Plan B® remain relatively expensive in the U.S.; Plan B® typically costs between $35 and $60, and the generic option is priced about 10% lower. Use of emergency contraception in the U.S. is very low compared to other modern contraceptives, and only 25% of OB/GYNs reported that they “routinely discuss” emergency contraception with their patients.(57)
Extended and Continuous Contraception
Since the FDA approved the first combined oral contraceptive, Enovid®, in 1960, the majority of oral hormonal contraceptives have followed a 21/7 cycle, in which the first 21 pills contain hormones, while the next seven pills are inactive (hormone-free).(58) During the inactive days, follicular growth resumes and the lining of the uterus is no longer maintained, so withdrawal bleeding occurs. Because there is no medical necessity for the withdrawal bleeding period, and because women have increasingly expressed interest in having fewer or no periods, a number of hormonal contraceptives have been developed that reduce or eliminate the hormone-free period.(59) Yasmin®, approved by the FDA in 2001, follows a 24/4 cycle, while extended (84/7) cycle oral contraceptives, such as Seasonale® and Seasonique®, reduce the number of withdrawal bleeds to only four per year.(60)(61)(62) Lybrel®, approved by the FDA in 2007, is a continuous contraceptive, which means it contains only active pills, so that bleeding is reduced or completely prevented (amenorrhea). Other methods of continuous contraception include hormonal implants and hormonal IUDs. Although some follicular growth occurs with continuous contraception, multiple studies have shown that continuous contraceptives suppress follicular growth more effectively than cyclical contraceptives, which may decrease the risk of ovulation and pregnancy.(63)
However, there are often disparities between provider and patient attitudes toward menstrual suppression. In 2004, 73% of American women surveyed were not aware that combined oral contraceptives could be used to skip a monthly period, while 81% of providers surveyed were aware that continuous contraception was available.(64) A 2003 study in Nigeria reported that although 73% of women surveyed expressed an interest in trying continuous contraception to induce amenorrhea, only 52% of providers surveyed would recommend continuous contraceptives.(65)
Male Contraception
In a review of male contraception research, Hoesl et al. (2005) reported that while cross-cultural surveys have revealed male and female interest in male contraception, reversible male contraceptive methods remain limited to condoms, abstinence, and coitus interruptus. The authors stipulate that reversible male contraceptives must be “as effective and safe as female methods with a fast onset of infertility and complete restoration of fertility after withdrawal, free of negative effects on offspring, [and] financially affordable, non-obtrusive, and convenient.”(66) Hormonal male contraception has been the most thoroughly researched method of male contraception. Recent clinical trials have evaluated the contraceptive potential of testosterone and a variety of synthetic hormones. Currently, androgen-progestin regimens have been the most promising hormonal method in terms of effectiveness and minimization of side effects.(67) Current challenges in male hormonal contraception include undesirable side effects and ethnic differences in contraceptive effectiveness; male hormonal contraceptives that have been successful in clinical trials with Asian populations have been much less effective in Caucasian populations.(68)
Non-hormonal methods studied recently often work by preventing sperm production with chemicals that affect activity in the testes or by blocking movement of sperm through the vas deferens.(69) For instance, RISUG (reversible inhibition of sperm under guidance) is a contraceptive injection that is being launched in India. The injection contains a polymer gel that damages sperm when inserted into the vas deferens, producing infertile sperm until reversed by a second injection. This procedure could cost as little as $10 and is 98% effective.(70)
Progress in male contraceptive research has been slowed by funding reductions. Between 2003 and 2008, three large international pharmaceutical companies stopped funding male contraception research, although funding continues to be provided by the World Health Organization, the Bill & Melinda Gates Foundation, and other public agencies.(71) The retreat of pharmaceutical companies from male contraception research may be attributable to “perceived poor profitability in the context of a shrinking global market” and concerns over lawsuits if new contraceptive methods fail.(72) Reengaging pharmaceutical companies that have lost interest in male hormonal contraception may help increase funding and facilitate research on a larger scale.
New Contraceptive Technologies(72)
Although advances in male contraceptive technologies have been slow, a review of developments in contraception by Rowlands (2009) describes a number of new female contraceptives that have recently been approved or are still in the testing phase. Many of these technologies are long-term contraceptives, and some have been found to be imperceptible to male partners, which could increase women’s control over preventing pregnancy and sexually transmitted diseases.
One recent innovation that could greatly increase contraceptive access in low- and middle-income countries is the Sayana Press. An injection that enters the skin rather than the muscle, the Sayana Press is extremely user-friendly and requires only basic training to administer; thus, community health workers and even laywomen themselves can inject the contraceptive. Like other injectable contraceptives, the Sayana Press is effective for three months, and it costs less than $1 per dose. Nearly 500,000 doses of were administered between 2014 and 2016 in the four countries that were part of the pilot initiative, and now several countries worldwide are incorporating the Sayana Press into their family planning programs.(74)
A number of researchers are investigating the possibility of oral contraceptives that do not use synthetic estrogens, which may decrease the very small risk of blood clots associated with hormonal contraceptives. Theoretically, estrogen-free contraceptives may also reduce the risk of breast cancer compared to estrogen-containing contraceptives, although the American Society for Reproductive Medicine reports, “there is no evidence of any increase in lifetime risk of breast cancer among [oral contraceptive] users.”(75) Estradiol (E2) and mifepristone have both shown promise as alternatives to ethinylestradiol, the most commonly used synthetic estrogen. In addition, pilot studies have suggested that self-injection of monthly contraceptives is effective and feasible. Progestogen-only rings have been developed as a contraceptive for women who are lactating and want an estrogen-free contraceptive; one such ring that is effective for up to four months is currently available in Chile and Peru.
Biodegradable subdermal implants are being researched as a long-lasting contraceptive that does not need to be removed, eliminating the possibility of complicated removals and the need for a visit to a health professional to perform the extraction. Early-stage studies have also investigated gel and spray contraceptives as alternatives to visible transdermal patches. In addition, frameless IUDs have been developed to minimize blood loss and pain, but their insertion requires specific training and a high level of medical competency. Early-stage studies have also evaluated the efficacy of adding microbicidal properties to spermicides, which may help reduce the risk of contracting sexually transmitted diseases. Studies have also found that male partners could not notice spermicide, which may be “potentially empowering to women whose partners will not use condoms.” In addition, barrier contraceptives developed based on feedback from users has led PATH (the Program for Approved Technology in Health) to develop the SILCS diaphragm, a “single-size, non-latex diaphragm with a polymer spring,” which reportedly fits most women without an assessment by a medical professional, is more comfortable than diaphragms with metal springs, and may be used with spermicides or lubricants. PATH also developed a female condom that can be inserted more easily and that does not move during use, which has resulted in promising levels of acceptability among women.
Further research and more funding are needed to enable the development of effective, low-cost methods of contraceptives for men and women. One large source of funding for new contraceptive technologies is the Gates Foundation, the world’s largest philanthropic organization, which has begun a $4 billion campaign to provide contraceptive access to 120 million more women by 2020. In May 2012, Melinda Gates announced that the foundation would be making family planning a priority, with an emphasis on developing innovative contraceptive methods, including self-injections and hormone-free birth-control pills. In July 2012, the Foundation co-sponsored a summit of world leaders in London to begin fundraising for its family planning initiative.(76)(77)
Abortions
When contraception is not used, unplanned pregnancy often results. Of the 85 million unintended pregnancies in 2012, half were voluntarily terminated.(78) Lack of access to safe abortion services often leads women to undergo unsafe abortions.(79) An unsafe abortion is “a procedure for terminating an unwanted pregnancy either by persons lacking the necessary skills or in an environment lacking the minimal medical standards, or both.”(80) Of the 22 million unsafe abortions each year, 87% occur in low- and middle-income countries, resulting in 47,000 deaths. (81) More than half of all abortions performed in low- and middle-income countries are considered unsafe; in Africa and Latin America, 95% of abortions are unsafe. Additionally, cultural stigma impacts medical professionals’ response to abortion complications; one study found that “the estimated mean time between diagnosis and initiation of treatment for women with abortion-related complications was 23.7 hours, compared with 1.2 hours for women with postpartum hemorrhage or eclampsia.”(82) These barriers to accessing medical care associated with improperly performed abortions can result in long-term health problems or death.
Conclusion
The cost of fully implementing basic family planning and reproductive health services, excluding HIV/AIDS, was estimated to be at least $14 billion in 2005, rising to $24.5 billion by 2015.(83) For $3.9 billion per year, contraceptive services could be extended to an additional 200 million women. The health benefits of spacing and limiting births for mothers and children are well known. Provision of family planning also has economic benefits, increasing the cost-effectiveness of such interventions. Ultimately, all women have the right to a safe pregnancy and childbirth, and all individuals and couples have the right to plan their families.
Footnotes
(1) World Health Organization. Maternal Mortality Fact Sheet. http://www.who.int/mediacentre/factsheets/fs348/en/.
(2) Ahmed, S., Li, Q., Liu, L., Tsui, A. 2012. Maternal Deaths averted by contraceptive use: an analysis of 172 countries. Lancet 380:111-125.
(3) United Nations International Conference on Population and Development. Reproductive rights and reproductive health. Programme of action of the United Nations ICPD. 1994. http://www.unfpa.org/publications/international-conference-population-and-development-programme-action.
(4) United Nations Department of Economic and Social Affairs. 2015. Trends in Contraceptive Use Worldwide. http://www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf.
(5) Marston, C. 2004. The effects of contraception on obstetric outcome. Geneva: World Health Organization. http://apps.who.int/iris/bitstream/10665/42949/1/9241592257.pdf.
(6) Adapted from http://www.usaid.gov/our_work/global_health/pop/index.html.
(7) Adapted from Planned Parenthood’s “How Pregnancy Happens.” https://www.plannedparenthood.org/learn/pregnancy/how-pregnancy-happens.
(8) Adapted from Planned Parenthood’s “Birth Control.” https://www.plannedparenthood.org/learn/birth-control.
(9) World Health Organization (WHO). 2017. “Family Planning Fact Sheet.” http://www.who.int/mediacentre/factsheets/fs351/en/.
(10) Planned Parenthood. “Birth Control”. https://www.plannedparenthood.org/learn/birth-control.
(11) Aetna. “Birth Control”.
(12) World Health Organization. “Family Planning/Contraception.” http://www.who.int/mediacentre/factsheets/fs351/en/.
(13) Ibid.
(14) Guttmacher Institute. November 2010. “Facts on Satisfying the Need for Contraception in Developing Countries.” http://www.a-id.org/pdf/facts-on-satisfying-the-need-for-contraception-in-developing-countries.pdf.
(15) United Nations Department of Economic and Social Affairs. 2015. Trends in Contraceptive Use Worldwide. http://www.un.org/en/development/desa/population/publications/pdf/family/trendsContraceptiveUse2015Report.pdf.
(16) Population Reference Bureau. 2008. Family planning worldwide: 2008 data sheet. Accessed on 11 August 2017 at http://www.prb.org/Publications/Datasheets/2008/familyplanningworldwide.aspx.
(17) Ahmed, S., Li, Q., Liu, L., Tsui, A. 2012. Maternal Deaths averted by contraceptive use: an analysis of 172 countries. Lancet. 380:111-125.
(18) Cleland J, Bernstein S, Ezeh A, Foundes A, Glasier A, Innis J. 2006. Family planning: the unfinished agenda. Lancet. 368:1810-27.
(19) Population Reference Bureau. 2013. Family planning worldwide: 2013 data sheet. http://www.prb.org/Publications/Datasheets/2013/family-planning-worldwide-2013.aspx.
(20) Ibid.
(21) Please visit http://www.uniteforsight.org/global-health-delivery-challenges/module2 for a discussion of attitudes towards family planning in Uganda and http://www.uniteforsight.org/global-health-delivery-challenges/module2b for a discussion of misconceptions about contraception among low-income Latina adolescents in the United States.
(22) Nalwadda, G., Mirembe, F., Byamugisha, J., Faxelid, E. (2010). Persistent high fertility in Uganda: young people recount obstacles enabling factors to use of contraceptives. BNC Public Health, 10:530.
(23) Nalwadda, G., Mirembe, F., Tumwesigye, N.M., Byamugisha, J., Faxelid, E. (2011). Constraints and prospects for contraceptive service provision to young people in Uganda: providers’ perspectives. BMC Health Serv. Res., 11:220.
(24) Ehrle, N., Sarker, M. (2011). Emergency contraceptive pills: knowledge and attitudes of pharmacy personnel in Managua, Nicaragua. Int Perspect Sex Reprod Health, 37(2): 67-74.
(25) Hubacher, D., Olawo, A., Manduku, C., Kiarie, J., Chen, P. (2012). Preventing unintended pregnancy among young women in Kenya: prospective cohort study to offer contraceptive implants. Contraception, 86.5 (2012): 511-517.
(26) Medhanie, AA et al. 2017. Factors associated with contraceptive use in Tigray, North Ethiopia. Reprod Health. 14(1):2.
(27) Glasier, A., Scorer, J., Bigrigg, A. (2008). Attitudes of women in Scotland to contraception: a qualitative study to explore the acceptability of long-acting methods. J Fam Plann Reprod Health Care, 34(4): 213-217.
(28) Guttmacher Institute. “Facts on Satisfying the Need for Contraception In Developing Countries”. November 2010. http://www.a-id.org/pdf/facts-on-satisfying-the-need-for-contraception-in-developing-countries.pdf.
(29) Ibid.
(30) Kristof, N.D. 19 May 2010. “Poverty and the Pill.” The New York Times. http://www.nytimes.com/2010/05/20/opinion/20kristof.html.
(31) Glasier, A.F., Smith, K.B., van der Spuy, Z.M., Ho, P.C., Cheng, L., Dada, K., Wellings, K., Baird, D.T. (2003). Amenorrhea associated with contraception- an international study on acceptability. Contraception, 67(1): 1-8.
(32) den Tonkelaar, I., Oddens, B.J. (1999). Preferred frequency and characteristics of menstrual bleeding in relation to reproductive status, oral contraceptive use, and hormone replacement therapy use. Contraception, 59:357-362.
(33) Bhatt, R., Bhatt, M. (2005). Perceptions of Indian women regarding menstruation. International Journal of Gynecology and Obstetrics, 88: 164–167.
(34) Please see http://www.uniteforsight.org/gender-power/module1, “Women Prevented From Accessing Health Care” for more information on the effects of family power dynamics and gender roles on women’s health.
(35) Guttmacher Institute. November 2010. “Facts on Satisfying the Need for Contraception In Developing Countries.” http://www.a-id.org/pdf/facts-on-satisfying-the-need-for-contraception-in-developing-countries.pdf.
(36) Hubacher, D., Olawo, A., Manduku, C., Kiarie, J., Chen, P. (2012). Preventing unintended pregnancy among young women in Kenya: prospective cohort study to offer contraceptive implants. Contraception, 86.5 (2012): 511-517.
(37) Nalwadda, G., Mirembe, F., Tumwesigye, N.M., Byamugisha, J., Faxelid, E. (2011). Constraints and prospects for contraceptive service provision to young people in Uganda: providers’ perspectives. BMC Health Serv. Res., 11: 220.
(38) Muanda, M., et al. Barriers to Modern Contraceptive Use in Kinshasa, DRC. 2016. PLoS One. 11(12):e0167560.
(39) Adapted from: Population Division, Department of Economic and Social Affairs, United Nations Secretariat. 25 April 2003. “Fertility, contraception, and population policies.” http://www.un.org/esa/population/publications/contraception2003/Web-final-text.PDF.
(40) Guttmacher Institute. 2020. “State Policies in Brief: Insurance coverage of contraceptives.” https://www.guttmacher.org/state-policy/explore/insurance-coverage-contraceptives.
(41)“Contraception and Insurance Coverage (Religious Exemption Debate).” 21 May 2012. The New York Times. https://www.nytimes.com/topic/subject/contraception-and-insurance-coverage.
(42) Landler, M. “Obama says he’s confident health care law will stand.” 3 April 2012. The New York Times. http://www.nytimes.com/2012/04/03/us/politics/obama-says-hes-confident-health-care-law-will-stand.html.
(43) Pear, R. “White House Acts to Roll Back Birth-Control Mandate for Religious Employers.” 29 May 2017. The New York Times. https://www.nytimes.com/2017/05/29/us/politics/birth-control-trump-obamacare-religion.html.
(44) Melnick, M. “Should the pill be sold over the counter?” Newsweek. 7 July 2010. http://www.newsweek.com/should-pill-be-sold-over-counter-74695.
(45) Landau, S.C., Tapias, M.P., McGhee, B.T. (2006). Birth control within reach: a national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception, 74(6): 463-470.
(46) WHO. “Emergency Contraception.” June 2017. Retrieved on11 August 2017 at http://www.who.int/mediacentre/factsheets/fs244/en/.
(47) The American Society for Reproductive Medicine. (2008). Hormonal contraception: recent advances and controversies. Fertility and Sterility, 90(3): 103-113.
(48) The Kaiser Family Foundation. “Fact Sheet: Emergency Contraception”. August 2016. http://www.kff.org/womens-health-policy/fact-sheet/emergency-contraception/.
(49) WHO. “Emergency Contraception”. June 2017. http://www.who.int/mediacentre/factsheets/fs244/en/.
(50) The Kaiser Family Foundation. “Fact Sheet: Emergency Contraception”. August 2016. http://www.kff.org/womens-health-policy/fact-sheet/emergency-contraception/.
(51) Brache, V., Croxatto, H., Sitruk-Ware, R., Maguire, R., Montero, J. C., Kumar, N., ... & Lahteenmaki, P. (2007). Effect of a single vaginal administration of levonorgestrel in Carraguard® gel on the ovulatory process: a potential candidate for “dual protection” emergency contraception. Contraception, 76(2), 111-116.
(52) International Consortium for Emergency Contraception. “EC Status and Availability.” http://www.cecinfo.org/country-by-country-information/status-availability-database/.
(53) Ibid.
(54) Ibid.
(55) Relph, M.K. “In India, Banking on the ‘Morning After’ Pill.” 26 May 2010. Time. http://content.time.com/time/world/article/0,8599,1991879,00.html.
(56) Ehrle, N., Sarker, M. (2011). Emergency contraceptive pills: knowledge and attitudes of pharmacy personnel in Managua, Nicaragua. Int Perspect Sex Reprod Health, 37(2): 67-74.
(57) Kliff, S. “Plan B’s Complicated History.” 24 August 2009. Newsweek. http://www.newsweek.com/plan-bs-complicated-legacy-78777.
(58) PBS Online. “American Experience: The Pill- Timeline”. 2002. http://www.pbs.org/wnet/need-to-know/health/a-brief-history-of-the-birth-control-pill/480/.
(59) Gladwell, M. “John Rock’s Error”. 10 March 2000. The New Yorker. http://www.newyorker.com/magazine/2000/03/13/john-rocks-error-2.
(60) Bayer Health Care Pharmaceuticals. “Yasmin®”. 2010.
(61) United States Food and Drug Administration. “FDA Approves Seasonale Oral Contraceptive”. 2003.
(62) Teva Women’s Health. “Seasonique®”. 2010.
(63) Birtch, R.L., Olufemi, A.O., Pierson, R.A. (2005). Ovarian follicular dynamics during conventional vs. continuous oral contraceptive use. Contraception, 73:235-243.
(64) Andrist, L.C., Arias, R.D., Nucatola, D., Kaunitz, A.M., Musselman, Reiter, S., Boulanger, J., Dominguez, L., Emmert, S. (2004). Women’s and providers’ attitudes toward menstrual suppression with extended use of oral contraceptives. Contraception, 70:359-363.
(65) Glasier, A.F., Smith, K.B., van der Spuy, Z.M., Ho, P.C., Cheng, L., Dada, K., Wellings, K., Baird, D.T. (2003). Amenorrhea associated with contraception- an international study on acceptability. Contraception, 67:1-8.
(66) Hoesl, C.E., Saad, F., Poppel, M., Altwein, J.E. (2005). Reversible, non-barrier male contraception: status and prospects. European Urology, 48: 712-723.
(67) Liu, P.Y., McLachlan, R.I. (2008). Male hormonal contraception: so near and yet so far. J Clin Endocrinal Metab, 93:2474–6.
(68) Hoesl, C.E., Saad, F., Poppel, M., Altwein, J.E. (2005). Reversible, non-barrier male contraception: status and prospects. European Urology, 48: 712-723.
(69) Cheng, C.Y., Mruk, D.D. (2011). Male contraception: Where do we go from here? Spermatogenesis, 1(4): 281-282.
(70) Altstedter, A. “A New Kind of Male Birth Control is Coming.” Bloomberg. 29 March 2017. https://www.bloomberg.com/news/features/2017-03-29/a-new-kind-of-male-birth-control-is-coming.
(71) Page, S.T., Amory, J.K., Bremner, W.J. (2008). Advances in male contraception. Endocr Rev, 29(4): 465-493.
(72) Liu, P.Y., McLachlan, R.I. (2008). Male hormonal contraception: so near and yet so far. J Clin Endocrinal Metab, 93:2474–6.
(73) Rowlands, S. (2009). New technologies in contraception. BJOG, 116(2): 230-9.
(74) PATH Reproductive Global Health Program. “Subcutaneous DMPA (Sayana Press): Expanding contraceptive access and options.” http://sites.path.org/rh/recent-reproductive-health-projects/sayanapress/?_ga=2.161716412.1831605522.1502391212-410600197.1502391212.
(75) The American Society for Reproductive Medicine. (2008). Hormonal contraception: recent advances and controversies. Fertility and Sterility, 90(3): 103-113.
(76) Goldberg, M. “Melinda Gates’ New Crusade: Investing Billions in Women’s Health”. 7 May 2012. Newsweek. http://www.newsweek.com/melinda-gates-new-crusade-investing-billions-womens-health-64965.
(77) Bill & Melinda Gates Foundation. “Family Planning: Strategy Overview.” https://www.gatesfoundation.org/What-We-Do/Global-Development/Family-Planning.
(78) Sedgh, G., Singh, S., Hussain, R. 2014. Intended and unintended pregnancies worldwide in 2012 and recent trends. Studies in Family Planning. 45:301-314.
(79) Glasier A, Gulmezoglu A, Schmid G, Moreno C, Van Look P. 2006. Sexual and reproductive health: a matter of life and death. Lancet. 368:1595-607.
(80) Grimes D, Benson J, Singh S, Romero M, Ganatra B, Okonofua F, et al. 2006. Unsafe abortion: the preventable pandemic. Lancet. 368:1908-19.
(81) World Health Organization. 2011. Unsafe abortion: global and regional estimates of the incidence of unsafe abortion and associated mortality in 2008. http://www.who.int/reproductivehealth/publications/unsafe_abortion/9789241501118/en/.
(82) Ibid.
(83) USAID’s Funding Decision on Reproductive Health and Family Planning. http://www.hewlett.org/wp-content/uploads/2016/08/USAID_FPRH_Funding_Decisions_-_OHanlon_April_2009.pdf.